ST. LOUIS — The lawyers who sued to force Missouri to accept newly eligible Medicaid recipients said the state's Department of Social Services is breaking federal law by waiting to approve new applications.
In an internal video obtained by 5 On Your Side, Missouri's DSS Family Support Division Director Kim Evans said applications for newly eligible Missourians won't be processed until Oct. 1.
"The applications will sit there until we have the eligibility piece in, which would be Oct. 1," Evans said in the video. "The plan is we’ll give instructions to you. Staff will go ahead and do the verification needed on the applications, but what we will do, we will not run a determination, we will not finalize these applications."
Chuck Hatfield with Stinson Law in Jefferson City partnered with the Legal Services of Eastern Missouri, or LSEM, to help three newly eligible women sue the state. On Thursday, the lawyers who led that legal battle — which forced the state to move ahead with the voter-approved expansion — said this expected delay violates federal law and goes against the judges ruling from earlier this month.
"The Court explicitly enjoined the Family Support Division and the rest of the Department of Social Services from prohibiting newly eligible individuals from enrolling in the MO HealthNet program," the lawyers said in a letter to Missouri's solicitor general. "Allowing individuals to submit applications is not the same as enrolling these individuals."
The federal Medicaid Act requires applications be processed within 45 days.
The letter was also sent to Kim Evans, Missouri DSS leaders and the director of Medicaid expansion, also known as MO HealthNet. In the letter, lawyers said they would prefer to resolve the issues outside of court but were prepared to "apprise the Court of these developments."
The state has said that qualifying health care costs that are incurred by eligible Missourians between the time they apply and when DSS is able to verify their eligibility may be reimbursed at a later date.
But Hatfield said that won't help many of the new recipients.
"A lot of these people just simply don't have the money to come out of their pocket and pay for it, so it's not very helpful to say, we will pay you back later if you don't have the cash today," Hatfield said.
Missouri's Medicaid expansion impacts 275,000 Missourians.
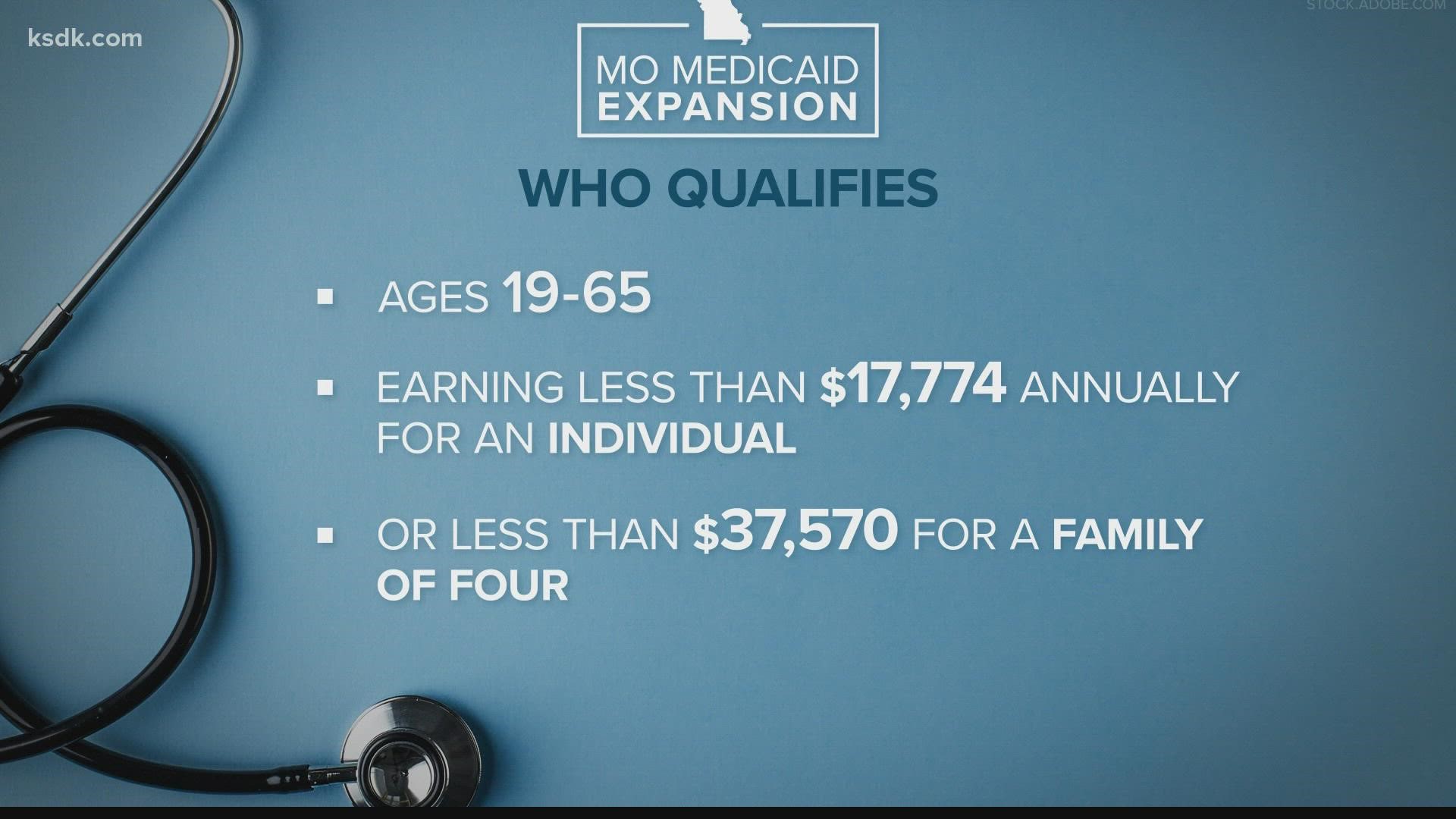
Those eligible include those earning up to 138% of the federal poverty level, including individuals ages 19-65 making less than $17,774 annually, or less than $37,570 for a family of four.
Apply on the DSS website.
How we got here
In August 2020, 53% of Missourians voted in favor of Medicaid expansion. It was supposed to take effect on July 1, 2021.
In February 2020, Gov. Parson and DSS sent the Centers of Medicare and Medicaid Services a state plan explaining, the state would move forward with the expansion.
DSS estimated the cost, and Parson included the suggested funds in his annual budget proposal to the General Assembly.
However, several Republicans argued it would cause the state to pay for an expensive program and result in a financial blow for future budgets.
On May 7, 2021, the legislature did not include the funding for the expansion in this year's budget. That's when Governor Parson said, without the money, they couldn't expand Medicaid.
The Lawsuit
On July 1, 2021, three women who were newly eligible for Medicaid were refused. They filed a lawsuit.
Melinda Hille was one of the plaintiffs. She was diagnosed with diabetes five years ago and has been fighting for her life.
The Missouri Supreme Court agreed with the voter-approved plan to stay in place, claiming the money is there.
The state Supreme Court ruled it did not violate the Missouri Constitution because it "does not appropriate money and does not remove the General Assembly's discretion in appropriating money to MO HealthNet."
On Aug. 11, a judge followed the ruling from the Missouri Supreme Court and issued an immediate injunction prohibiting the state from denying enrollment to the expanded population or treating them differently.
That day, Governor Parson released a statement and said, "My administration is always going to follow the law."
That press release said the system update is anticipated to take up to 60 days because of limited staffing and funding.
It explained they are working through administrative hurdles, including adequate appropriations, staffing capacity, and computer software changes in order to begin enrolling the expanded population.
Since the proposed funds were not included in this year's budget, DSS is limited to administering the expanded program without sufficient staffing or money.
In order to comply with the court order, DSS is reassigning existing employees from their current assignments in order to evaluate applications.
In addition, qualifying health care costs that are incurred by eligible Missourians between the time they apply and when DSS is able to verify their eligibility may be reimbursed at a later date.
Hille is one of the people who doesn't want to rack up more bills.
"There is no way I will be able to crawl out of this financial hole. I can’t afford hundreds of thousands of dollars that I’ve racked up over the years. A lot of people have put their health on the back burner they don’t want to run up their bills," she said. "The more they put this off, the more illnesses they get. Every day counts for a lot of people."
Even if the state will not review applications until Oct. 1, Hatfield wants to be clear: Get an application on file right now, if you are eligible.
"It's going to be paid for by Medicaid even though you may not get your eligibility determination for a couple of weeks," he said. "The providers are going to go ahead and give you the treatment, knowing they're going to be paid by Medicaid.
"Go into your clinic, your pharmacy or doctor, whatever it is, tell them you're Medicaid eligible and they'll help you through the process and make sure you get the care you need."
Hatfield said he is concerned about a potential backlog.
"If they get 100,000 applications, I don't think they're going to be able to flip a switch and have all 100,000 people determined to be eligible on that day," he said. "There are always issues with Medicaid applications. There is always a back and forth in the process to make sure the state has the right information. The cycle of waiting till Oct. 1, really for a lot of people means you're waiting until mid-October, or maybe even longer, as they work their application through the process."