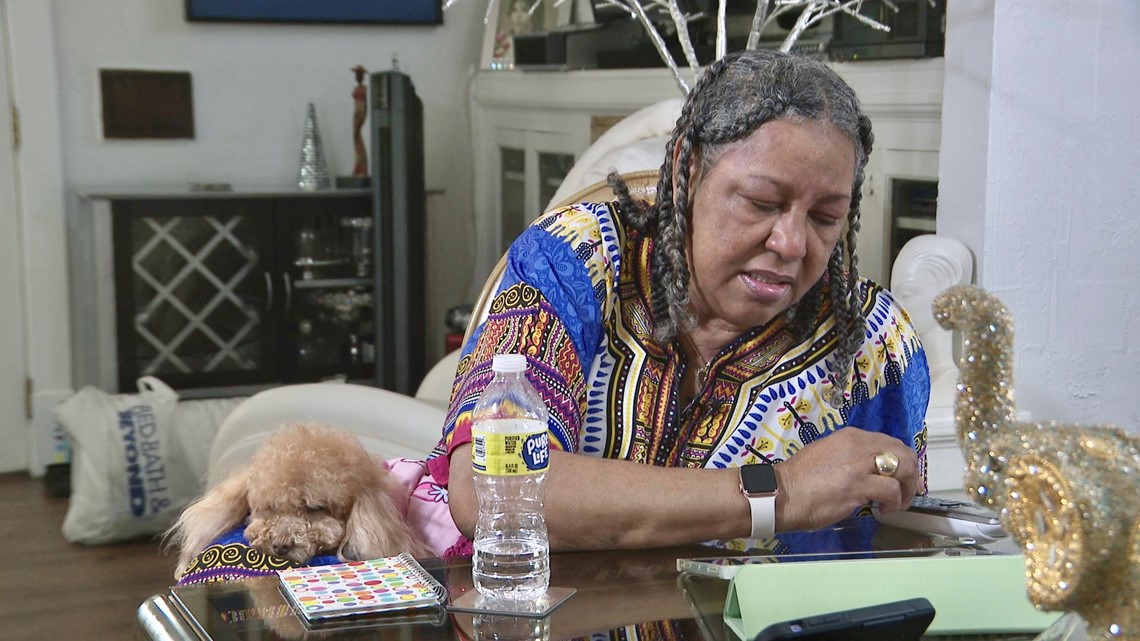
ST. LOUIS — North St. Louis resident Troy Gardner just couldn't log in.
"I don't know why I can't do it, but I can't... I'm just over it... I'm so sick of this, this is giving me a headache," Gardner said.
"If you were able to go to the doctor from the comfort of your home, how would that impact your life?" asked the I-Team's Paula Vasan.
"Oh, it would be wonderful," she said.
Gardner, 66, wanted to change her next doctor's visit to an online appointment because getting there in person is painful.
"I'm just torn up, just nerve damage everywhere," she said.
She has the option.
"I got the iPad, and I have my phone," she said.
She doesn't have the skills.
"It's truly frustrating," said Gardner.

Gardner is one of many impacted by the digital divide, which refers to the gap between those who have access to digital technology and those who don't. These technologies include smartphones, computers and the internet. Many researchers say one area where the digital divide is most impactful is health care.
There are efforts to close the gap. The Biden administration has announced new commitments from 20 internet providers to help close the digital divide gap by lowering the cost of high-speed internet for millions of people. But many industry experts argue that’s only one aspect of closing the digital divide. Many people lack access to broadband and technological devices like computers and smartphones to go online. Researchers say other people lack the skills or confidence to use that technology, while others don't know how to access resources to help them learn or are hesitant to do so.
Researchers say the "digital divide" is more common among people in their 60s and older. They're often the ones who need to see their doctors the most. A study done at the start of the pandemic estimated one in three older adults in the U.S. had trouble visiting their doctor online. And it's still a problem.
In April, a St-Louis-based report showed access to high-speed internet, affordability of devices, and understanding how to use technology all contribute to a very deep digital divide. They found the main drivers are coverage, quality, affordability, and digital literacy.
The report was commissioned by the St. Louis Community Foundation and the Regional Business Council and prepared by the Center for Civic Research and Innovation and the accounting firm Ernst & Young. The report showed that between 250,000 to 300,000 households in St. Louis City and St. Louis County lack access to fiber internet service. About 90,000 households across the City and County cannot afford adequate devices. And 25% of households in the City do not have a computer or only have a smartphone.
"It's a systemic problem in this country," said Amy VanDeVelde, director at The Oasis Institute, a nonprofit that works with BJC HealthCare and other health systems nationwide. Her goal: To help people like Gardner learn how to use telehealth and email their doctors. She can't keep up.


"So it's a really big problem," said VanDeVelde. "I am a staff of one."
She said the program gets about $50,000 a year in funding.
"It's minimal. It's not enough," she said.
She said the program needs about 20 times the amount of funding it gets to operate effectively and help people like Troy Gardner, who had never heard of the program.


Following our interview with Gardner, the I-Team took 25 minutes to figure out why Gardner couldn't get into her patient portal.
"I'm not stupid. If you teach me how, then I can," said Gardner.
After she reset her password and downloaded the correct app, she was finally able to log in. She said she'll be making more virtual appointments.
"I don't know what to say. I can't believe we're in," said Gardner.
Gardner's first telehealth appointment could be sometime in May. We'll check in to see how it went. We also spoke with some of the biggest health care systems in our area about how they're responding to the need for online appointments and training.
A spokesperson with BJC Healthcare tells us that before the pandemic, less than 1% of appointments were online. At the peak of the pandemic, that number went up to 30%. Today, around 5% of appointments are telehealth appointments.
A BJC spokesperson said in an email: “BJC HealthCare is committed to improving access to care and services that promote good health. Several programs are designed to enable access – including a remote monitoring program for St. Louis Children’s Hospital’s high-risk pediatric cardiology patients; a program through BJC Behavioral Health that provides up to six months of unlimited phone, text and internet services; in-home virtual visit support in certain Barnes Jewish Hospital clinics; and educational support through BJC’s Oasis program. BJC and Washington University School of Medicine also developed a home monitoring program for patients with COVID-19.”
A spokesperson with Mercy told us it will take many stakeholders such as public health, lawmakers, insurance companies and health systems working together to address the digital divide. In an email, they told us: “Since the beginning of the pandemic, Mercy has provided more than 800,000 virtual visits between patients and Mercy Clinic medical providers, a stark increase from the 10,000 Mercy virtual visits in 2019… The average monthly number across all of Mercy is about 20,000 video visits.”
We asked what percentage of patients request telehealth but are unable to do it because of failing technology. A spokesperson with Mercy told us: “Unfortunately, we have no way to measure failures at this time. Often when a connection fails for a video visit, it’s quickly converted to a telephone visit and the patient gets the care they need immediately. We do strongly encourage reporting of these issues and do offer troubleshooting guides to try help as much as possible, but time is a factor as well.”
Erin Powell, SSM Health’s system vice president of digital health told us: “Like many organizations, we have worked hard to expand available services and make telehealth/virtual care more accessible to all. On top of having multiple options for telehealth services we also have services that are accessible without insurance and at a low retail cost. Our goal is to ensure that these services are accessible to all.”
We asked what obstacles SSM has noticed in providing care during the pandemic in a more virtual world. “We found we had to pivot quickly to meet the needs of the community and fast change never comes without some difficulty. Staff, providers, and patients had to adjust to a new process and a new way of receiving and delivering care,” said Powell.
In terms of what groups of people have experienced the most significant obstacles when it comes to access to health care in a more digital world, she said the largest obstacles always come to those that don’t have accessibility to the internet and technology. “There can also be significant struggles for those that are less comfortable leveraging technology as a solution. Finding assistance to learn can be difficult,” she said. “We are still working to see how we can assist in helping those that don’t have access to the internet or even the technology to utilize these services. We realize that these offerings can be crucial to providing healthcare in rural and underserved areas of our communities.”
In response to how SSM’s number of telehealth appointments have been impacted during the pandemic, Powell said: “Pre-COVID on average we were doing about 9,000 visits per year as a system. At the height of the pandemic in 2020 we did just over 570,000. We slowed down considerably in 2021 completing just over 308,000. We expect 2022 to be much like 2021. We have found that the community and providers have adopted and really come to like the convenience and ease of utilizing Virtual health as an option for care.”
RESOURCES:
The Oasis Institute, based in St. Louis, is a nonprofit that promotes healthy aging through lifelong learning, active lifestyles and volunteer engagement. Its services also include digital literacy. To learn more about the Oasis Institute’s technology-training services: https://connections.oasisnet.org/ . You can also call 314-687-4525.
If you’d like to help support The Oasis Institute and its mission to teach digital literacy, you can donate by visiting www.oasisnet.org/donate. You can also call 314-862-2933 extension 240 or send an email to lreichardt@oasisnet.org.

