JEFFERSON CITY, Mo. — As millions of Medicaid recipients face the potential loss of health coverage for the first time since the coronavirus pandemic, state call centers are getting inundated with questions from people needing help. In some cases, federal officials say, it’s taking too long to get answers.
Nearly one-third of the states have received warnings from federal Medicaid officials that their lengthy call center wait times may be causing people to hang up — and give up — as they attempt to renew Medicaid coverage amid a massive nationwide effort to clean up the rolls of the government health insurance program for lower-income residents.
Some advocates have offered to function like placeholders in a long line for concert or sports tickets — waiting on hold so Medicaid recipients can do other things.
“If you call a call center and you have a sort of significant wait, you oftentimes are neglecting your work duties, you’re neglecting needs of your family, otherwise growing impatient," said Matt Slonaker, executive director of the Utah Health Policy Project, a nonprofit that assists Medicaid recipients. "What we’ve seen anecdotally over and over again is people giving up.”
Utah had an average call center wait time of 35 minutes in May, with one in four callers simply hanging up, according to the federal Centers for Medicare and Medicaid Services.
According to the most recent CMS data, the longest wait time was in Missouri, at 48 minutes, though state officials say that figure is misleading. In Nevada, more than half the callers abandoned their calls.
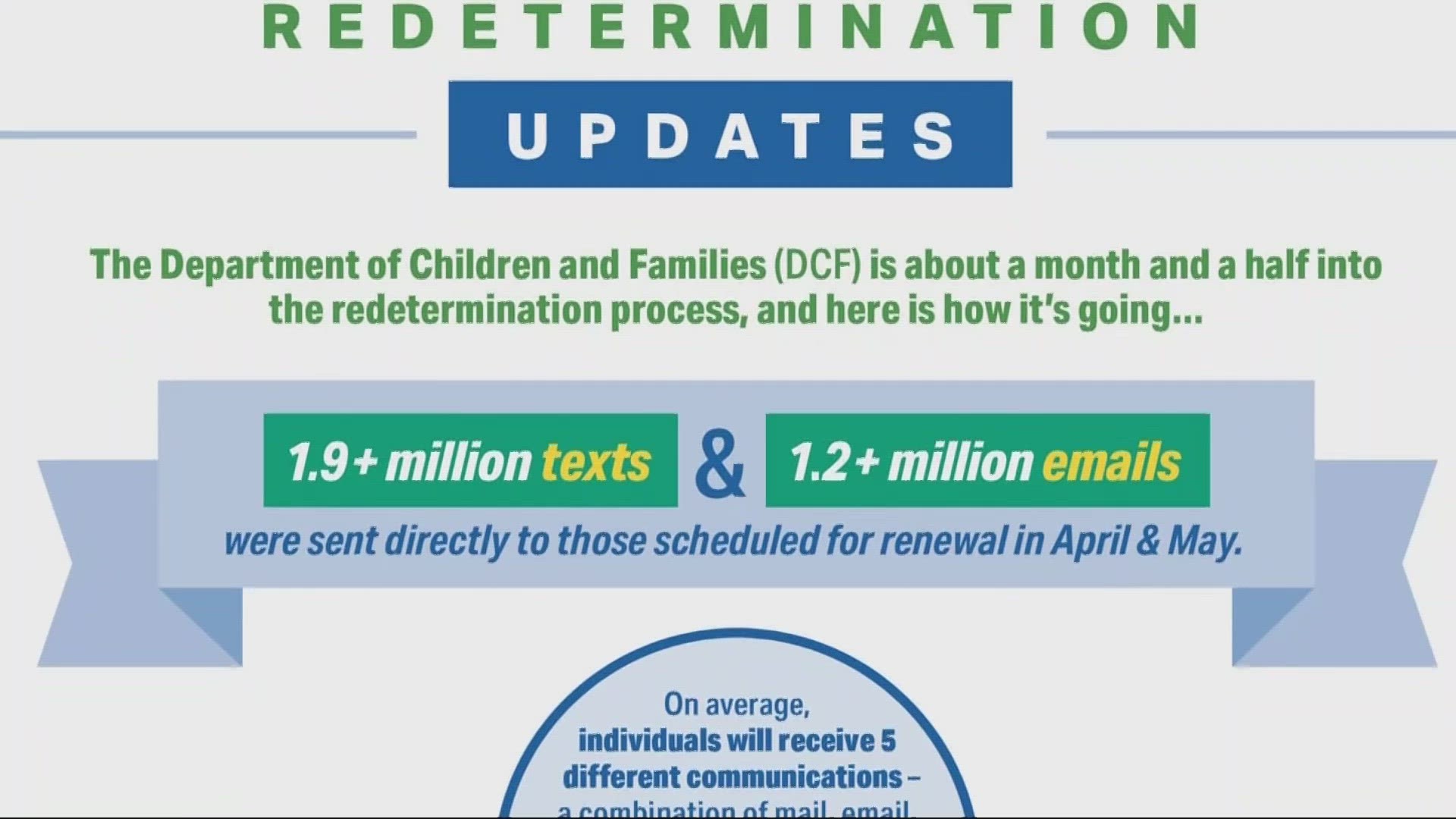
States typically conduct annual eligibility reviews. But they are now dealing with a backlog of cases because the federal government prohibited states from removing people from Medicaid during the coronavirus pandemic — a roughly three-year moratorium that ended in April.
During that time, Medicaid enrollment swelled by nearly one-third, from 71 million people in February 2020 to 94 million in April 2023.
Since then, well over 4 million people have lost Medicaid coverage during the mandatory renewal process. Most of those people were dropped for what CMS describes as procedural reasons, such as failing to return renewal forms.
In letters sent last week to state Medicaid agencies, CMS raised concerns that long call center wait times and high abandonment rates “are impeding equitable access to assistance and the ability for people to apply for or renew Medicaid” and may run afoul of federal requirements. Similar warnings were sent to 16 states — Alaska, Arizona, Florida, Hawaii, Idaho, Illinois, Kansas, Maine, Missouri, Montana, Nevada, New Mexico, Oregon, Rhode Island, South Carolina and Utah.
Among those 16 states, the average call center wait time was 25 minutes and the average hang-up rate was 29%. That's significantly higher than the rest of the states, where the average call wait was less than 3 minutes and the average hang-up rate was less than 6%.
Though many states added staff or contractors to help handle the surge in eligibility determinations, some state Medicaid officials acknowledged difficulty in keeping up with the calls.
“For sure it has been a challenge,” said Dave Baden, interim director of the Oregon Health Authority. "With the amount of humanity we’re going through, there’s no way we could have hired up so many people to be ready for all of that.”


In some states, the same staff who make Medicaid eligibility determinations also are responsible for fielding phone calls.
“It is a tradeoff. We can’t process applications as fast if we put more people on the phones,” said Jeanne Lambrew, commissioner of the Maine Department of Health and Human Services.
Utah has faced a similar balancing act in splitting staff time between answering phones and processing Medicaid renewals, said Nate Checketts, deputy director of the Utah Department of Health and Human Services. Within a few months, he said, the department hopes to have improved its computer capabilities to automatically renew some people based on data compiled for other social services programs such as food assistance.
"That will help cut down on the number of individuals that need to call us to try to clarify information on their forms,” Checketts said.
Missouri's nationally high May call center wait time of 48 minutes was based on data from a general call center, said state Department of Social Services spokesperson Caitlin Whaley. Revised data from four call centers that take Medicaid calls show an average wait time of 28 minutes in May, she said.
But Missouri has taken several steps since to drive down wait times, including having whoever answers the phone address all of a caller's needs instead of potentially transferring the caller to multiple people, Whaley said. The department also has adopted “a blitz strategy” when many phones are ringing.
“During times of high call volume, it’s like an all-hands-on-deck,” she said, adding, "workers and supervisors both are answering calls to try and help more people and get those wait times down.”